

2975 Westchester Ave,
Suite G02
Purchase, NY 10577
(914) 902-5780
1177 Summer Street,
4th Floor
Stamford, CT 06905
(203) 614-8355
The person who has lost teeth regains the ability to eat virtually anything, knowing that teeth appear natural and that facial contours will be preserved. Patients with dental implants can smile with confidence.
For most patients, the placement of dental implants involves two surgical procedures. First, implants are placed within your jawbone. For the first three to six months following surgery, the implants are beneath the surface of the gums gradually bonding with the jawbone. You should be able to wear temporary dentures and eat a soft diet during this time. At the same time, your dentist is forming new replacement teeth.
After the implant has bonded to the jawbone, the second phase begins. Dr. Graffeo or Dr. Linsky will uncover the implants and attach small posts that protrude through the gums and will act as anchors for the artificial teeth. When the artificial teeth are placed, these posts will not be seen. The entire procedure usually takes six to eight months. Most patients experience minimal disruption in their daily life.
Dental Implant placement is a team effort between an oral and maxillofacial surgeon and a restorative dentist. While Dr. Graffeo and Dr. Linsky perform the actual implant surgery, initial tooth extractions, and bone grafting if necessary, the restorative dentist (your dentist) fits and makes the permanent prosthesis. Your dentist will also make any temporary prosthesis needed during the implant process.
To provide you with a better understanding of dental implants, we have provided the following multimedia presentation. Many common questions pertaining to dental implants are discussed.
Having trouble? Please make sure you have the Adobe Flash Player plugin installed in order to correctly view this presentation. This software is available as a free download.
A single prosthesis (crown) is used to replace one missing tooth – each prosthetic tooth attaches to its own implant. A partial prosthesis (fixed bridge) can replace two or more teeth and may require only two or three implants. A complete dental prosthesis (fixed bridge) replaces all the teeth in your upper or lower jaw. The number of implants varies depending upon which type of complete prosthesis (removable or fixed) is recommended. A removable prosthesis (over denture) attaches to a bar or male- female attachments, whereas a fixed prosthesis is permanent and removable only by the dentist.
Dr. Graffeo and Dr. Linsky perform in-office implant surgery in a hospital-style operating suite, thus optimizing the level of sterility. Inpatient hospital implant surgery is for patients who have special medical or anesthetic needs or for those who need extensive bone grafting from the jaw, hip or tibia.
Once you learn about dental implants, you finally realize there is a way to improve your life. When you lose several teeth – whether it’s a new situation or something you have lived with for years – chances are you have never become fully accustomed to losing such a vital part of yourself.
Dental implants can be your doorway to renewed self-confidence and peace of mind.
A Swedish scientist and orthopedic surgeon, Dr. Per-Ingvar Branemark, developed this concept for oral rehabilitation more than 35 years ago. With his pioneering research, Dr. Branemark opened the door to a lifetime of renewed comfort and self-confidence for millions of individuals facing the frustration and embarrassment of tooth loss.
There are several reasons: Why sacrifice the structure of surrounding good teeth to bridge a space? In addition, removing a denture or a “partial” at night may be inconvenient, not to mention that dentures that slip can be uncomfortable and rather embarrassing.
If you are considering implants, your mouth must be examined thoroughly and your medical and dental history reviewed. If your mouth is not ideal for implants, ways of improving outcome, such as bone grafting, may be recommended.
The majority of dental implants and bone graft can be performed in the office under local anesthesia, with or without general anesthesia.
Once the implants are in place, they will serve you well for many years if you take care of them and keep your mouth healthy. This means taking the time for good oral hygiene (brushing and flossing) and keeping regular appointments with your dental specialists.
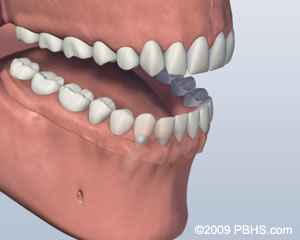
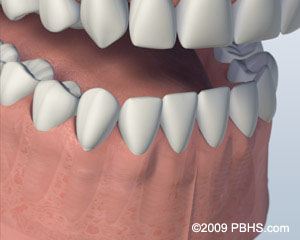
As you rely more on your remaining teeth, you increase the chance they will wear out prematurely, or be damaged or lost. You may also experience headaches and/or jaw pain. Who would want their appearance and health to deteriorate? That’s the natural consequence of missing teeth – the jaw literally melts away.
Generally, people will lose 25% of their supporting jawbone structure within the first year after tooth loss. Dental implants are more easily placed when teeth are first extracted because bone replacement becomes more complex as time passes. The great news? Implants act just like your natural teeth. They safeguard and preserve your bone structure, oral health and appearance. Your dentist and the implant surgeon will provide you with options so that you can make the most informed decision concerning tooth replacement.
You can select from a number of different options to replace your missing teeth – from temporary to long-lasting solutions.
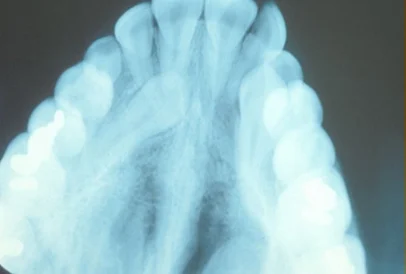
A good candidate is anyone missing one or more teeth, or who is unhappy with their dentures. Age is not a factor. However, smoking, diseases such as diabetes, and radiation therapy to the area, have been shown to lower the success rate of implant placement. X-rays of your jaw will be taken to evaluate whether they will accommodate implants. Detailed x-rays may also be required to determine if other tests or procedures are needed to place implants properly.

A fixed bridge is a connected set of replacement teeth. For support, it is cemented into position on top of the teeth adjacent to the empty space. The protective outer layer of these teeth is usually removed or ground down prior to attaching the bridge.

A fragile, temporary and inexpensive solution is a removable plastic tooth with a plastic retainer, often called a “flipper”.

A less fragile option is a removable partial denture cast in metal and plastic. It is held in place by wire clips. A removable partial denture can be removed and reinserted when required by the patient.
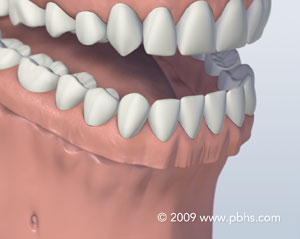
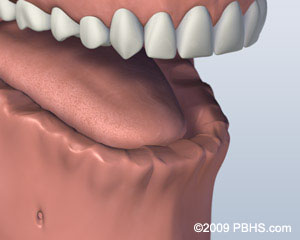
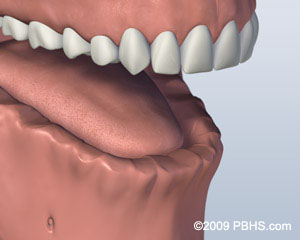
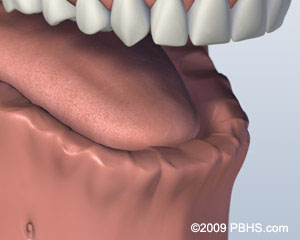
The most common solution, for people missing all teeth in one or both jaws are complete dentures. Some people adapt well to dentures. Others find them uncomfortable, even intolerable, because of differences in jaw size and shape.

Dental implants are the most comfortable and permanent solution. They form a strong foundation for teeth and keep the jaw healthy and strong. Implants support individual replacement teeth or secure specialized dentures in place. Unlike bridges, no healthy teeth are damaged. Unlike most bridges, implants can last a lifetime. Implant-supported replacement teeth can be attractive, stable, and comfortable for almost any patient.
To provide you with a better understanding of dental implants, we have provided the following multimedia presentation. Many common questions pertaining to dental implants are discussed.
Having trouble? Please make sure you have the Adobe Flash Player plugin installed in order to correctly view this presentation. This software is available as a free download.
There are several reasons: A dental bridge can sacrifice the structure of surrounding good teeth to bridge the space of the missing tooth/teeth. In addition, removing a denture or a “partial” at night may be inconvenient, not to mention dentures that slip can be uncomfortable and rather embarrassing.
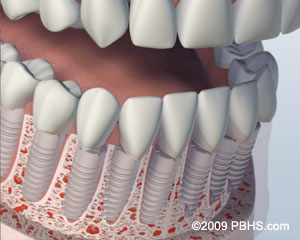
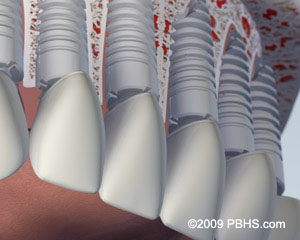
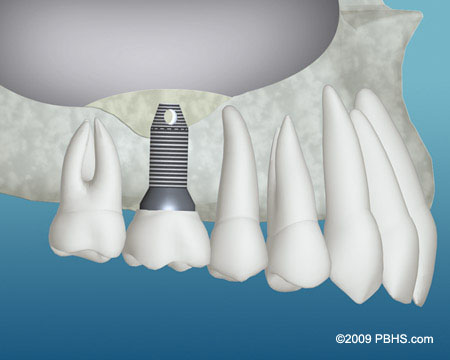
A natural tooth consists of a root and a crown. If you compare natural teeth to implant-supported replacement teeth, you’ll see they have the same basic parts. Both have a crown (the visible part used to chew food). Both have a root that holds the tooth securely under the gum and is anchored into the jaw. The difference is that the implant is made of titanium – the same time-tested material used by surgeons for artificial joints. When you lose a tooth, you lose both the root and the crown. To replace the tooth, the surgeon first replaces the root with a small dental implant.
Time is allowed for bone to heal and grow around the dental implant. The bone bonds with the titanium, creating a strong foundation for artificial teeth. A support post (abutment) is then placed on the implant and a new replacement tooth (crown) is placed on top of the abutment. In many cases a temporary replacement tooth can be attached to the implant immediately after it is placed. If all of your teeth are missing, a variety of treatment options are available to support the replacement teeth.
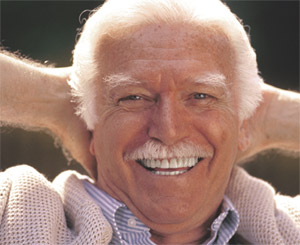
For years I’d felt like a part of my body was missing — because my teeth were. My dentist told me that dental implants would make me feel and look a lot better. OK, I said. Now, I’m thrilled. I can smile, eat anything, and enjoy a good laugh with my friends.
Using the most recent advances in dental implant technology, Dr. Graffeo and Dr. Linsky are able to place single stage implants. These implants do not require a second procedure to uncover them, but do require a minimum of six weeks of healing time before artificial teeth are placed. There are even situations where the implant can be placed at the same time as the tooth extraction – further minimizing your number of surgical procedures.
Dental implant placement is a team effort between an oral and maxillofacial surgeon and a restorative dentist. Dr. Graffeo and Dr. Linsky perform the actual implant surgery, initial tooth extractions, and bone grafting if necessary. The restorative dentist (your dentist) fits and makes the permanent prosthesis. Your dentist will also make any temporary prosthesis needed during the implant process.
Both have a crown (the visible part used to chew food). Both have a root that holds the tooth securely under the gum and is anchored into the jaw. The difference is that the implant is made of titanium – the same time-tested material used by surgeons for artificial joints. When you lose a tooth, you lose both the root and the crown. To replace the tooth, the surgeon first replaces the root with a small dental implant.
Time is allowed for bone to heal and grow around the dental implant. The bone bonds with the titanium, creating a strong foundation for artificial teeth. A support post (abutment) is then placed on the implant and a new replacement tooth (crown) is placed on top of the abutment. In many cases a temporary replacement tooth can be attached to the implant immediately after it is placed. If all of your teeth are missing, a variety of treatment options are available to support the replacement teeth.
The procedure to place an implant takes 30 to 60 minutes for one implant and only 2 to 3 hours for multiple implants. The number of appointments and time required, vary from patient to patient. The surgeon will bring great precision and attention to the details of your case.
Prior to surgery, you may receive antibiotics and for greater comfort, intravenous sedation or nitrous oxide (laughing gas). These options are discussed with you at your consultation appointment. A local anesthetic will be administered to numb the area where the implant will be placed.
When you are comfortable, the surgeon makes a small incision in the gum tissue to reveal the bone, creates space using special instruments, and gently inserts the titanium implant. The top of this implant is often visible through the gum. Sometimes it is better in the early stages of healing to have the implant covered by the gum tissue.

1. Normal

2. Tooth Loss

3. Healed Bone

4. Implant Placed

5. Healing

6. Implant Restored
Now the healing begins. The length of time varies from person to person, depending upon the quality and quantity of bone. In some cases, implants may be restored immediately after they are placed. The surgeon will advise you on follow-up care and timing. After the initial phase of healing, the surgeon places an abutment (support post) or a healing cap onto the implant during a brief follow-up visit. This allows gum tissue to mature and provides access to the implant.
Occasionally, impressions are made at the time the implant is placed. This enables the crown to be ready when the implants have healed. How long your mouth needs to heal is determined by a variety of factors. Follow-up care (one to four appointments) is usually needed to ensure that your mouth is healing well and to determine when you are ready for the restorative phase of your treatment.
It may be beneficial to perform a soft tissue graft to obtain stronger, more easily cleaned and natural appearing gum tissue in the area around the implant. This process involves moving a small amount of gum tissue from one part of your mouth to the area around the implant. Most often, it is a brief and relatively comfortable procedure.
Whether it’s one tooth or all of your teeth that are being replaced, your dentist will complete the restoration by fitting the replacement tooth (crown) to the dental implant.
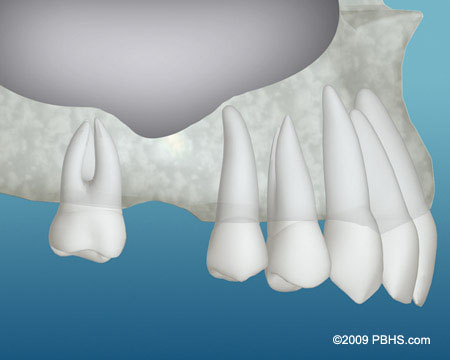
Implants are often placed several months after extraction. At times, an implant may be placed immediately after extraction of a tooth. This may involve a little more risk, but it simplifies the process—you won’t have to wait for another appointment to place the implant. When infection or other problems with the bone are present, immediate implant placement is not the best treatment.
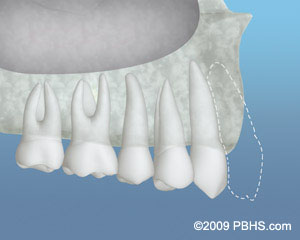
If your tooth has been missing for some time, the adjacent support bone is likely to grow thinner and shrink. This occurs because the root of the natural tooth has to be present to stimulate the bone. As much as one third of your jaw’s thickness can be lost in the year following tooth extraction. If you are missing enough bone, you may benefit from having additional bone grafted into the area. This ensures the implant will be adequately supported when it is placed in the jaw.
Most frequently, one implant per missing tooth is placed. Because many of the larger teeth in the back of your jaws have two or three roots, the most common approach is to replace missing back teeth with larger implants.
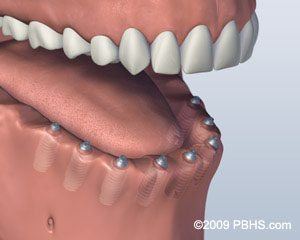
One option is to have two implants placed in your lower jaw and a denture made that snaps onto these implants. This option allows your lower denture to be more stable while chewing than without implants. However, there will still be movement of your lower denture, and sore spots will occur if any food particles, especially seeds, are caught under it. As with all removable replacement teeth, you still will need periodic appointments for denture adjustment.
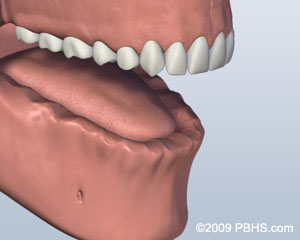
1. Before
2. Implants Placed
3. Denture Attached
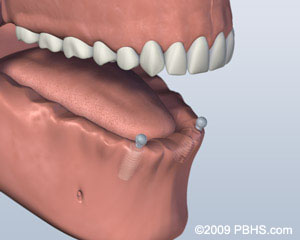
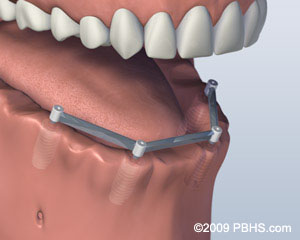
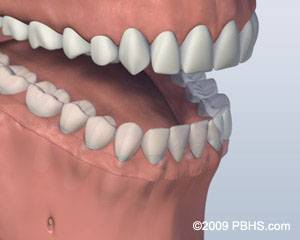
Another option involves placing four to six implants, depending on your jaw size or shape, into your lower jaw. After healing is complete, the implants are connected with a custom-made support bar. Your denture will be made with special internal retention clips that attach onto the support bar, enabling the denture to snap firmly into place. This is called an “overdenture.” The advantage of this option is that it is much more stable than the first option and allows very little denture movement. Your denture is still removable for easy cleaning and maintenance.
1. Before
2. Implants Placed
3. Denture Attached
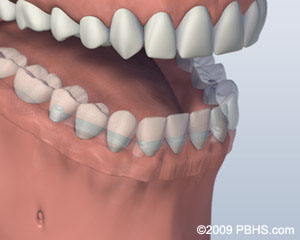
A third option involves placing five or more implants in your jaw and attaching a permanent denture. Your denture is held in place by screws or clasps that secure it to the support posts or bar. It doesn’t touch the gum tissue, which allows you to clean under the denture without removing it. This denture will replace all your missing lower teeth and will not be removed except at maintenance visits. Although cleaning under your denture without removing it is more time consuming and requires more dexterity, many patients who want a permanent denture prefer this option.
1. Before
2. Implants Placed
3. Denture Attached
The final option is to have all your teeth individually replaced so that they will appear to be growing out of your gum tissue and will most closely resemble the appearance of your natural teeth. This option usually requires eight or more implants. Separate abutments or support posts for each one of these implants will be made and crowns for each missing tooth will be placed. The teeth are often joined together for sinus grafting to replace bone height strength and support. Overall, this is the most costly option, because it requires the most implants and individual replacement tooth fabrication. Your replacement options may also be limited by the current size and shape of your jawbone.
1. Before
2. Implants Placed
3. Denture Attached
A similar range of treatment options is also available for your upper jaw. However, because the bone is not as hard as that in the lower jaw, people often need more implants to support their new replacement teeth. Depending upon the number of implants to be placed, it may be possible to eliminate the need for covering the roof of your mouth with a complete denture. This option allows you to fully taste your food and gives you a better sense of its temperature. Your denture will feel more natural. You will still have a removable denture, which makes cleaning the support bar and denture much easier.

Depending upon the number of implants to be placed, it may be possible to eliminate the need for covering the roof of your mouth with a complete denture. This option allows you to fully taste your food and gives you a better sense of its temperature. Your denture will feel more natural. You will still have a removable denture, which makes cleaning the support bar and denture much easier.
If you want a restoration that is similar to your natural teeth and therefore not removable, you probably will need eight to ten individual implants placed. This is followed after healing by the placement of the abutments and new replacement crowns.
After tooth extraction, if the walls of the socket are very thick, they will usually fill naturally with bone in two to three months. However, when the walls of your socket are very thin (such as in your upper and lower front teeth), this type of healing will not be as predictable. In these situations, a bone graft is often placed at the time of tooth extraction to help your body fill in the empty socket with bone. This step will maintain the width and volume of bone you will need for implant placement several months later.
1. Inadequate Bone
2. Graft Material Placed

3. Implants Placed
There may be inadequate bone for implant placement if your tooth was removed many years ago and your bony ridge is extremely thin. In this case, a bone graft can be placed next to the thin bone and allowed to heal for up to six months. After the graft has fused to your pre-existing bone, the ridge will be re-entered and the implant placed. Bone grafting is usually a relatively comfortable office procedure. Many different bone-grafting materials are available, including your own bone.
1. Inadequate Bone
2. Graft Material and Implant Placed
You may also need bone grafting if the sinus cavities in your upper jaw are very large, or very low, and extend into the tooth-bearing areas. This often occurs when teeth in the back of a person’s upper jaw have been removed many years before, and the amount of bone available for implant placement is limited. A “sinus grafting procedure” is then required. Most often, it is performed in the office with local anesthesia and perhaps sedation. During this procedure, the membrane that lines the sinus will be located and elevated. Bone will then be added to restore the bone height and ensure that dental implants of an adequate length can be placed. This procedure often can be performed at the time of implant placement.
The Bar Attachment Denture is a contemporary restoration that has revolutionized the way surgeons and dentists think of replacing a full set of teeth. Standard dentures are unsecured prostheses with inherent limitations. Most often, dentures are painful, inconvenient and unstable. Such dentures can make chewing foods difficult, limiting the foods that you once enjoyed.
Fortunatley, modern dentistry can help with Bar Attachment Denture implant-supported dentures. The Bar Attachment Denture treatment concept replaces your missing teeth with a full dental bridge supported by only four dental implants. With fewer implants needed, overall treatment time and cost is reduced. The unique Bar Attachment Denture solution also ensures greater stability in the bone, reducing the need for bone graft surgery to increase bone volume.
After a short healing period, your dentist will place the final bridge. Your quality of life is improved, and you can start enjoying your favorite foods again with renewed confidence.
Scientifically proven and documented. Bar Attachment Denture is supported by good clinical outcomes from studies over a decade with favorable results.
TEETH-IN-AN-HOUR™ is a revolutionary concept providing patients with fully functioning teeth on dental implants in a single procedure that takes about an hour. This technology was developed by Nobel Biocare and utilizes collaboration between both the restorative doctor and the oral surgeon. This merging of knowledge and experience achieves not only increased safety, but also a more precise implant placement.
The fabrication of a final prosthesis is completed prior to the surgery. The computer-guided implant surgery is done in an arthroscopic fashion without requiring any flap reflection. This benefits the patient in that there is less postoperative discomfort, less swelling, and less bruising. Patients can often resume their normal activities the next day.
The process begins when a CAT scan is taken of the patient’s jawbone. This CAT scan allows for the generation of a three-dimensional model of the jawbone that can then be used with virtual reality software to plan the implant placement without the presence of the patient. The results are a more accurate implant placement and less chair time for the patient.

Although it is natural to be concerned about the pain that may be caused by these procedures, most patients do not experience severe or significant post-operative pain. Pain medication and antibiotics will be prescribed for you to make your recovery as easy as possible. Occasionally, some people develop post-operative infections that require additional antibiotic treatment. Even though great care is taken to place the implant precisely, occasionally adjacent teeth are injured in the placement process. In addition, there is a chance that the nerve in the lower jaw, which provides sensation to your lower lip and chin, may be affected. If you are missing quite a lot of bone, it might be difficult to place an implant without infringing on the nerve space. Although we take great care to avoid this nerve, occasionally it is irritated during the procedure, resulting in tingling, numbness or a complete lack of sensation in your lip, chin or tongue. Usually these altered sensations will resolve within time, but they can be permanent and/or painful. If you notify us of post-operative numbness as soon as possible, it will allow us to manage your care in the most appropriate way.
Implants usually last a long time. When patients are missing all of their teeth, long-term studies (more than 30 years) show an 80 to 90 percent success rate. For patients missing one or several teeth, recent studies show a success rate of greater than 95 percent, which compares favorably with other areas in the body that receive implant replacement (such as hips or knees). However, if one of your dental implants either doesn’t heal properly or loosens after a period of time, you may need to have it removed. After the site heals (or on occasion at the time of removal), another implant usually can be placed.
The replacement teeth are usually attached to the implant when adequate healing has occurred and your jawbone is firmly fused to the implant. Depending on a variety of factors, it may be possible to begin this phase of your treatment immediately or shortly after implant placement. We will review the most appropriate treatment sequence and timing for your particular situation.
The dental work required to complete your treatment is complex. Most of the work involves actually making the new teeth before they are placed. Your appointments are considered more comfortable and more pleasant than previous methods of tooth replacement. Frequently, this process can be performed without local anesthesia.
Your restorative treatment begins with specialized impressions that allow us to produce a replica of your mouth and implants. We will also make “bite” records so that we see the relationship of your upper and lower jaws. With this information, we will make the abutments (support posts) that attach your replacement teeth to your implants. Various types of abutments exist. Frequently, we can use “off the shelf” abutments. Other times, custom abutments must be made of gold or a tooth-colored ceramic material. As you can imagine, these custom made abutments add to the cost and treatment time involved. Which abutment to use is a decision that often cannot be made until after healing is complete and impressions have been made.
The number of appointments and the amount of time required for each appointment is different for each patient. No two cases are exactly the same and regardless of the number of teeth replaced, the work must be completed with great precision and attention to detail. If you are having only a few teeth replaced, as few as three short appointments may be required. Between appointments, we will need time to complete the necessary lab work to make your replacement teeth. It is most beneficial that you keep all of your scheduled appointments.
If your final restoration is a removable denture, you will need to come to as many as five office appointments (although it may be fewer) over the following several months. During these appointments, we will perform a series of impressions, bites and adjustments in order to make your new teeth, as well as the custom support bars, snaps, magnets, or clips that will secure your teeth to the implants. During this period, every effort will be made to ensure you have comfortable, temporary replacement teeth.
In general, once your implants are placed, you can expect your tooth replacement treatment to be completed anywhere from 1 to 12 months. For these reasons, it is difficult for us to tell you exactly how much the restorative phase of your treatment will cost, although you should receive a reasonable estimate from our office. It also is difficult to give you a specific timeframe for completion of your treatment until after the implants are ready for restoration.

are the most technologically advanced and longest lasting tooth replacement option available. Restore your confidence… Smile, Eat and Enjoy!
As with natural teeth, it is important that you clean implant-supported restorations regularly with toothbrushes, floss and any other recommended aids. You should also visit your dentist several times each year for hygiene and maintenance. As with regular dentures and other tooth replacements, your implants and their associated components are subject to wear and tear and eventually will need repair, including clip replacement, relines, screw tightening, and other adjustments.
Usually, a dental surgeon places the implant(s) and performs other necessary surgical procedures – your general dentist provides the temporary and permanent replacement teeth. Both doctors are involved in planning your dental treatment. Also, depending upon a variety of factors, different dental specialists may help with your dental care.
Before treatment begins, every effort will be made to give you an accurate estimate of all the expenses involved in placing the implants and making your replacement teeth. In many cases, there is an initial charge for the diagnostic work-up, including study models, x-rays, and the fabrication of a surgical template to ensure the best possible result. In addition you will be charged for the abutment or support post(s), plus the crown, dentures, or anything else that will be placed over the implants, including temporary restorations. Periodic maintenance such as hygiene visits, tissue conditioners, denture relines and other repairs will also incur additional charges.
When different doctors are involved in your treatment, you will be charged separately for their services. We will try to assist you in estimating what your actual payments will be after we evaluate your insurance coverage or other third party payments. Also, you should consider your personal financial investment in each treatment option as some insurance companies provide limited or no coverage.
Each patient is unique, and it is not possible for us to discuss every option and every contingency for treatment outcome. This booklet is intended to help you understand the general treatment options available to you. If your specific treatment options are not clear, please contact us. We will be happy to answer any questions you have about your dental care.
When comparing the cost of dental implants to other tooth replacement methods such as dentures and bridges, it is important to take into consideration the longevity offered by dental implants that is not always afforded by other, more traditional methods.
While dentures and bridges are initially less expensive, their affordability can be short-lived. Because these older methods require repair and replacement every 5-10 years, they are often more expensive over time. By contrast, dental implants, when properly placed and cared for, can last a lifetime.
Over time, when a tooth is missing, the jawbone deteriorates. So while a denture or bridge may seem to function similarly to a tooth, underneath the surface damage is being done to the jawbone and ultimately to the structure of the face. This can result in the distortion of the shape of a person’s face, leading to additional cosmetic costs down the road.
On the other hand, dental implants are made of titanium, which actually integrates with the jawbone, strengthening it and stimulating bone growth. This preserves the natural strength and quality of the mouth, lessening problems in the future.
Dental implants can be seen as a long-term investment not only in terms of money, but also in terms of quality of life. A dental implant is the closest thing to a natural tooth. In addition to allowing the patient to eat the same healthy foods he or she has always enjoyed, it also eliminates the day-to-day hassles and possible embarrassment that are frequently caused by dentures.
There are several steps (and often multiple professionals) involved in the placement of a dental implant. When comparing quotes, it’s important to factor in the cost of each of these steps:
First, check with your dental insurance carrier to see what portion, if any, of dental implants they cover.
There are health care credit companies that offer no-interest and low-interest loans for medical procedures including dental implants.
Dental Implants are an investment in your health as well as your appearance. A full set of teeth makes eating a pleasure again, making it easier to eat a balanced, healthy diet. A full set of teeth also preserves the contours of the face, keeping you from looking old before your time.
The only way to receive an accurate fee is to call us and come in for a consultation. While at our office we will review all of your options, formulate a treatment plan and present the fees. Please call us at (914) 902-5780 to schedule your consultation.
Over a period of time, the jawbone associated with missing teeth atrophies, or is reabsorbed. This often leaves a condition in which there is poor quality and quantity of bone suitable for placement of dental implants. In these situations, most patients are not candidates for placement of dental implants.
Today, we have the ability to grow bone where needed. This not only gives us the opportunity to place implant of proper length and width, it also gives us a chance to restore functionality and esthetic appearance.
Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease, or injuries. The bone is either obtained from a tissue bank or your own bone is taken from the jaw, hip, or tibia (below the knee.) Sinus bone grafts are also performed to replace bone in the posterior upper jaw. In addition, special membranes may be utilized that dissolve under the gum and protect the bone graft and encourage bone regeneration. This is called guided bone regeneration or guided tissue regeneration.
Major bone grafts are typically performed to repair defects of the jaws. These defects may arise as a result of traumatic injuries, tumor surgery, or congenital defects. Large defects are repaired using the patient’s own bone. This bone is harvested from a number of different sites depending on the size of the defect. The skull (cranium), hip (iliac crest), and knee (tibia) are common donor sites. These procedures are routinely performed in an operating room and require a hospital stay.
When one or more teeth are missing, it can lead to jawbone loss at the site of the gap. This loss of jawbone can develop into additional problems, both with your appearance and your overall health. You may experience pain, problems with your remaining teeth, and altered facial appearance, and eventually even the inability to speak and eat normally.
In that same way that muscles are maintained through exercise, bone tissue is maintained by use. Natural teeth are embedded in the jawbone, and stimulate the jawbone through activities such as chewing and biting. When teeth are missing, the alveolar bone, or the portion of the jawbone that anchors the teeth in the mouth, no longer receives the necessary stimulation, and begins to break down, or reabsorb. The body no longer uses or “needs” the jawbone, so it deteriorates and goes away.
With bone grafting, we now have the opportunity to not only replace bone where it is missing, but also the ability to promote new bone growth in that location! This not only gives us the opportunity to place implants of proper length and width, it also gives us a chance to restore functionality and aesthetic appearance.
Autogenous Bone Grafts:
Autogenous bone grafts, also known as autografts, are made from your own bone, taken from somewhere else in the body. The bone is typically harvested from the chin, jaw, lower leg bone, hip, or the skull. Autogenous bone grafts are advantageous in that the graft material is live bone, meaning it contains living cellular elements that enhance bone growth.
However, one downside to the autograft is that it requires a second procedure to harvest bone from elsewhere in the body. Depending on your condition, a second procedure may not be in your best interest.
Allogeneic Bone:
Allogeneic bone, or allograft, is dead bone harvested from a cadaver, then processed using a freeze-dry method to extract the water via a vacuum. Unlike autogenous bone, allogeneic bone cannot produce new bone on its own. Rather, it serves as a framework or scaffold over which bone from the surrounding bony walls can grow to fill the defect or void.
Xenogenic Bone:
Xenogeneic bone is derived from non-living bone of another species, usually a cow. The bone is processed at very high temperatures to avoid the potential for immune rejection and contamination. Like allogeneic grafts, xenogeneic grafts serve as a framework for bone from the surrounding area to grow and fill the void.
Both allogeneic and xenogeneic bone grafting are advantageous in that they do not require a second procedure to harvest your own bone, as with autografts. However, because these options lack autograft’s bone-forming properties, bone regeneration may take longer than with autografts, with a less predictable outcome.
As a substitute to using real bone, many synthetic materials are available as a safe and proven alternative, including:
Demineralized Bone Matrix (DBM)/Demineralized Freeze-Dried Bone Allograft (DFDBA):
This product is processed allograft bone, containing collagen, proteins, and growth factors that are extracted from the allograft bone. It is available in the form of powder, putty, chips, or as a gel that can be injected through a syringe.
Graft Composites:
Graft composites consist of other bone graft materials and growth factors to achieve the benefits of a variety of substances. Some combinations may include: collagen/ceramic composite, which closely resembles the composition of natural bone, DBM combined with bone marrow cells, which aid in the growth of new bone, or a collagen/ceramic/autograft composite.
Bone Morphogenetic Proteins:
Bone morphogenetic proteins (BMPs) are proteins naturally produced in the body that promote and regulate bone formation and healing.
Synthetic materials also have the advantage of not requiring a second procedure to harvest bone, reducing risk and pain. Each bone grafting option has its own risks and benefits. Drs. Graffeo and Linsky will determine which type of bone graft material is right for you.
The alveolar ridge of the jaw is the bone that surrounds the roots of teeth. When a tooth is removed, an empty socket is left in the alveolar ridge bone. Usually this empty socket will heal on its own, filling with bone and tissue. Sometimes when a tooth is removed, the bone surrounding the socket breaks, and it is unable to heal on its own. The previous height and width of the socket will continue to deteriorate.
Rebuilding the original height and width of the alveolar ridge is not medically necessary, but may be required for dental implant placement, or for aesthetic purposes. Dental implants require bone to support their structure, and a ridge augmentation can help rebuild this bone to accommodate the implant.
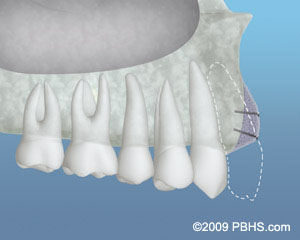
A ridge augmentation is accomplished by placing bone graft material in the tooth socket. It is often done immediately after the tooth is removed, to avoid the need for a second procedure later. Next, the gum tissue, or membrane(guided tissue regeneration) is placed over the socket and secured with sutures. Dr. Graffeo and Dr. Linsky may choose to use a space-maintaining product over the top of the graft to help restore the height and width of the space created by the tooth and bone loss, and into which new bone should grow. Once the socket has healed, the alveolar ridge can be prepared for dental implant placement.
A ridge augmentation procedure is typically performed in Dr. Graffeo and Dr. Linsky under local anesthesia. Some patients may also request sedative medication in addition.
The maxillary sinuses are behind your cheeks and on top of the upper teeth. These sinuses are empty, air-filled spaces. Some of the roots of the natural upper teeth extend up into the maxillary sinuses. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. Dental implants need bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
If bone loss has occurred due to injury or periodontal disease, a sinus augmentation can raise the sinus floor and allow for new bone formation. A sinus lift is one of the most common bone grafting procedures for patients with bone loss in the upper jaw. The procedure seeks to grow bone in the floor of the maxillary sinus above the bony ridge of the gum line that anchors the teeth in the upper jaw. By strengthening and growing bone in this location, dental implants can be placed and secured in the new bone growth.
A sinus lift may be necessary if you:
In the most common sinus augmentation procedure, a small incision is made on the premolar or molar region to expose the jawbone. A small opening is cut into the bone, and the membrane lining the sinus is pushed upward. The underlying space is filled with bone grafting material, either from your own body or from a cadaver. Sometimes, synthetic materials that can imitate bone formation are used. After the bone is implanted, the incision is stitched up and the healing process begins. After several months of healing, the bone becomes part of the patient’s jaw and dental implants can be inserted and stabilized in this new sinus bone.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant well, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for several months, depending upon the type of graft material used. Once the graft has matured, the implants can be placed.
The sinus graft makes it possible for many patients to have dental implants when years ago there was no other option besides wearing loose dentures.
A sinus augmentation is generally performed at Dr. Graffeo and Dr. Linsky’s office, under local anesthesia. However, some patients also may request oral or intravenous sedative medication as well.
In severe cases, the ridge has been reabsorbed and a bone graft is placed to increase ridge height and/or width. This is a technique used to restore the lost bone dimension when the jaw ridge gets too thin to place conventional implants. In this procedure, the bony ridge of the jaw is literally expanded by mechanical means. Bone graft material can be placed and matured for a few months before placing the implant.
The teeth in the front of the mouth (incisors, canine, and bicuspid teeth) are ideal for grasping and biting food into smaller pieces. The back teeth (molar teeth) are used to grind food up into a consistency suitable for swallowing.
The average mouth is made to hold only 28 teeth. It can be painful when 32 teeth try to fit in a mouth that holds only 28 teeth. These four other teeth are your third molars, also known as “wisdom teeth.”
Wisdom teeth are the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen. The extraction of wisdom teeth is necessary when they are prevented from properly erupting within the mouth. They may grow sideways, partially emerge from the gum, and even remain trapped beneath the gum and bone. Impacted teeth can take many positions in the bone as they attempt to find a pathway that will allow them to successfully erupt.
These poorly positioned impacted teeth can cause many problems. When they are partially erupted, the opening around the teeth allows bacteria to grow and will eventually cause an infection. The result: swelling, stiffness, pain, and illness. The pressure from the erupting wisdom teeth may cause damage to adjacent teeth. The most serious problem occurs when tumors or cysts form around the impacted wisdom teeth, resulting in the destruction of the jawbone and healthy teeth. Removal of the offending impacted teeth usually resolves these problems. Early removal is recommended to avoid such future problems and to decrease the surgical risk involved with the procedure.
With an oral examination and x-rays of the mouth, Dr. Graffeo and Dr. Linsky can evaluate the position of the wisdom teeth and predict if there are present or may be future problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid-teenage years by their dentist, orthodontist or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Dr. Graffeo and Dr. Linsky have the training, license and experience to provide various types of anesthesia for patients to select the best alternative.
To provide you with a better understanding of wisdom teeth, we have provided the following multimedia presentation. Many common questions pertaining to wisdom teeth are discussed.
Having trouble? Please make sure you have the Adobe Flash Player plugin installed in order to correctly view this presentation. This software is available as a free download.
In most cases, the removal of wisdom teeth is performed under local anesthesia, laughing gas (nitrous oxide/oxygen analgesia) or general anesthesia. These options, as well as the surgical risks (i.e., sensory nerve damage, sinus complications), will be discussed with you before the procedure is performed. Once the teeth are removed, the gum is sutured. To help control bleeding, bite down on the gauze placed in your mouth. You will rest under our supervision in the office until you are ready to be taken home. Upon discharge, your postoperative kit will include postoperative instructions, a prescription for pain medication, antibiotics, and a follow-up appointment in one week for suture removal. If you have any questions, please do not hesitate to call us at (914) 902-5780.
Our services are provided in an environment of optimum safety that utilizes modern monitoring equipment and staff who are experienced in anesthesia techniques.
An impacted tooth simply means that it is “stuck” and cannot erupt into function. These teeth get “stuck” in the back of the jaw and can develop painful infections among a host of other problems (see Impacted Wisdom Teeth under Procedures).
Since there is rarely a functional need for wisdom teeth (third molar teeth), they are usually extracted if they develop problems. The maxillary cuspid (upper eyetooth) is the second most common tooth to become impacted. The cuspid tooth is a critical tooth in the dental arch and plays an important role in your “bite”. The cuspid teeth are very strong biting teeth and have the longest roots of any human teeth. They are designed to be the first teeth that touch when your jaws close together so they guide the rest of the teeth into the proper bite.
Normally, the maxillary cuspid teeth are the last of the “front” teeth to erupt into place. They usually come into place around age 13 and cause any space left between the upper front teeth to close tighter together. If a cuspid tooth gets impacted, every effort is made to get it to erupt into its proper position in the dental arch. The techniques involved to aid eruption can be applied to any impacted tooth in the upper or lower jaw, but most commonly they are applied to the maxillary cuspid (upper eye) teeth.
Sixty percent of these impacted eyeteeth are located on the palatal (roof of the mouth) side of the dental arch. The remaining impacted eye teeth are found in the middle of the supporting bone but stuck in an elevated position above the roots of the adjacent teeth or out to the facial side of the dental arch.
Click image below for larger view





The older the patient, the more likely an impacted eyetooth will not erupt by nature’s forces alone even if the space is available for the tooth to fit in the dental arch. The American Association of Orthodontists recommends that a panorex screening x-ray, along with a dental examination, be performed on all dental patients at around the age of seven years to count the teeth and determine if there are problems with eruption of the adult teeth.
It is important to determine whether all the adult teeth are present or are some adult teeth missing. Are there extra teeth present or unusual growths that are blocking the eruption of the eyetooth? Is there extreme crowding or too little space available causing an eruption problem with the eyetooth? This exam is usually performed by your general dentist or hygienist who will refer you to an orthodontist if a problem is identified.
Treating such a problem may involve an orthodontist placing braces to open spaces to allow for proper eruption of the adult teeth. Treatment may also require referral to an oral surgeon for extraction of over-retained baby teeth and/or selected adult teeth that are blocking the eruption of the all-important eyeteeth. The oral surgeon will also need to remove any extra teeth (supernumerary teeth) or growths that are blocking eruption of any of the adult teeth. If the eruption path is cleared and the space is opened up by age 11-12, there is a good chance the impacted eyetooth will erupt with nature’s help alone.
If the eyetooth is allowed to develop too much (age 13-14), the impacted eyetooth will not erupt by itself even with the space cleared for its eruption. If the patient is too old (over 40), there is a much higher chance the tooth will be fused in position. In these cases the tooth will not budge despite all the efforts of the orthodontist and oral surgeon to erupt it into place. Sadly, the only option at this point is to extract the impacted tooth and consider an alternate treatment to replace it in the dental arch (crown on a dental implant or a fixed bridge).
In cases where the eyeteeth will not erupt spontaneously, the orthodontist and oral surgeon work together to get these unerupted eyeteeth to erupt. Each case must be evaluated on an individual basis but treatment will usually involve a combined effort between the orthodontist and the oral surgeon. The most common scenario will call for the orthodontist to place braces on the teeth (at least the upper arch). A space will be opened to provide room for the impacted tooth to be moved into its proper position in the dental arch. If the baby eyetooth has not fallen out already, it is usually left in place until the space for the adult eyetooth is ready. Once the space is ready, the orthodontist will refer the patient to the oral surgeon to have the impacted eyetooth exposed and bracketed.
In a simple surgical procedure performed in the surgeon’s office, the gum on top of the impacted tooth will be lifted up to expose the hidden tooth underneath. If there is a baby tooth present, it will be removed at the same time. Once the tooth is exposed, the oral surgeon will bond an orthodontic bracket to the exposed tooth. The bracket will have a miniature gold chain attached to it. The oral surgeon will guide the chain back to the orthodontic arch wire where it will be temporarily attached. Sometimes the surgeon will leave the exposed impacted tooth completely uncovered by suturing the gum up high above the tooth or making a window in the gum covering the tooth (on selected cases located on the roof of the mouth). Most of the time, the gum will be returned to its original location and sutured back with only the chain remaining visible as it exits a small hole in the gum.
Shortly after surgery (same day-14 days) the patient will return to the orthodontist. A rubber band will be attached to the chain to put a light eruptive pulling force on the impacted tooth. This will begin the process of moving the tooth into its proper place in the dental arch. This is a carefully controlled, slow process that may take up to a full year to complete. Remember, the goal is to erupt the impacted tooth and not to extract it! Once the tooth is moved into the arch in its final position, the gum around it will be evaluated to make sure it is sufficiently strong and healthy to last for a lifetime of chewing and tooth brushing. In some circumstances, especially those where the tooth had to be moved a long distance, there may be some minor “gum surgery” required to add bulk to the gum tissue over the relocated tooth so it remains healthy during normal function. Your dentist or orthodontist will explain this situation to you if it applies to your specific situation.
These basic principals can be adapted to apply to any impacted tooth in the mouth. It is not that uncommon for both of the maxillary cuspids to be impacted. In these cases, the space in the dental arch form will be prepared on both sides at once. When the orthodontist is ready, the surgeon will expose and bracket both teeth in the same visit so the patient only has to heal from surgery once. Because the anterior teeth (incisors and cuspids) and the bicuspid teeth are small and have single roots, they are easier to erupt if they get impacted than the posterior molar teeth. The molar teeth are much bigger teeth and have multiple roots making them more difficult to move. The orthodontic maneuvers needed to manipulate an impacted molar tooth can be more complicated because of their location in the back of the dental arch.
Recent studies have revealed that with early identification of impacted eyeteeth (or any other impacted tooth other than wisdom teeth), treatment should be initiated at a younger age. Once the general dentist or hygienist identifies a potential eruption problem, the patient should be referred to the orthodontist for early evaluation. In some cases the patient will be sent to the oral surgeon before braces are even applied to the teeth. As mentioned earlier, the surgeon will be asked to remove over-retained baby teeth and/or selected adult teeth.
He will also remove any extra teeth or growths that are blocking eruption of the developing adult teeth. Finally, he may be asked to simply expose an impacted eyetooth without attaching a bracket and chain to it. In reality, this is an easier surgical procedure to perform than having to expose and bracket the impacted tooth. This will encourage some eruption to occur before the tooth becomes totally impacted (stuck). By the time the patient is at the proper age for the orthodontist to apply braces to the dental arch, the eyetooth will have erupted enough that the orthodontist can bond a bracket to it and move it into place without needing to force its eruption. In the long run, this saves time for the patient and means less time in braces (always a plus for any patient!).
The surgery to expose and bracket an impacted tooth is a very straightforward surgical procedure that is performed in the oral surgeon’s office. For most patients, it is performed under IV sedation. The procedure is generally scheduled for 75 minutes if one tooth is being exposed and bracketed and 105 minutes if both sides require treatment. If the procedure only requires exposing the tooth with no bracketing, the time required will be shortened by about one half. These issues will be discussed in detail at your preoperative consultation with your doctor. You can also refer to Preoperative Instructions under Surgical Instructions on this website for a review of any details.
You can expect a limited amount of bleeding from the surgical sites after surgery. Although there will be some discomfort after surgery at the surgical sites, most patients find Tylenol or Advil to be more than adequate to manage any pain they may have. Within two to three days after surgery there is usually little need for any medication at all. There may be some swelling from holding the lip up to visualize the surgical site; it can be minimized by applying ice packs to the lip for the afternoon after surgery.
Bruising is not a common finding at all after these cases. A soft, bland diet is recommended at first, but you may resume your normal diet as soon as you feel comfortable chewing. It is advised that you avoid sharp food items like crackers and chips as they will irritate the surgical site if they jab the wound during initial healing. Your doctor will see you seven days after surgery to evaluate the healing process and make sure you are maintaining good oral hygiene. You should plan to see your orthodontist within the same day to 14 days post surgery to activate the eruption process by applying the proper rubber band to the chain on your tooth. As always your doctor is available at the office or called after hours if any problems should arise after surgery. Simply call Westchester Oral & Maxillofacial Surgery & Implantology at (914) 902-5780 if you have any questions.
An orthodontic TAD or Temporary Anchorage Device is a tiny dental implant that looks like a mini screw that’s temporarily placed through the gum tissue and into the jawbone. TADs are usually made of titanium alloy, which is a durable, safe, biocompatible material. Once the TADs are in place, they serve as an anchorage, which means they are a fixed point that can be used to provide force to shift the teeth in the desired direction. With breakthroughs like TADs, orthodontists can move teeth in ways that weren’t possible in the past, allowing us the ability to treat complex cases. They allow the orthodontist to create a customized system for exerting pressure that’s tailored to a patient’s needs. When the tooth movements have been achieved the TADs are removed. Some patients will have their temporary anchorage devices for several months, while others will have TADs for the duration of their orthodontic treatment.
Endodontic surgery can be used to locate fractures or hidden canals that do not appear on x-rays but still manifest pain in the tooth. Damaged root surfaces or the surrounding bone may also be treated with this procedure. The most common surgery used to save damaged teeth is an apicoectomy or root-end resection.
The above diagram illustrates this simple procedure. An incision is made in the gum tissue to expose the bone and surrounding inflamed tissue. The damaged tissue is removed along with a small amount of the root tip. A root-end filling is placed to prevent reinfection of the root and the gum is sutured. The bone naturally heals around the root over a period of months restoring full function.
Following the procedure, there may be some discomfort or slight swelling while the incision heals. This is normal for any surgical procedure. To alleviate any discomfort, an appropriate pain medication will be recommended. If you have pain that does not respond to medication, please call our office. We routinely see our surgery patients for a post-surgical check two weeks after surgery, and then again in six months for a recall examination.
The maxillary sinuses are behind your cheeks and on top of the upper teeth. These sinuses are empty, air-filled spaces. Some of the roots of the natural upper teeth extend up into the maxillary sinuses. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. Dental implants need bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
If bone loss has occurred due to injury or periodontal disease, a sinus augmentation can raise the sinus floor and allow for new bone formation. A sinus lift is one of the most common bone grafting procedures for patients with bone loss in the upper jaw. The procedure seeks to grow bone in the floor of the maxillary sinus above the bony ridge of the gum line that anchors the teeth in the upper jaw. By strengthening and growing bone in this location, dental implants can be placed and secured in the new bone growth.
A sinus lift may be necessary if you:
In the most common sinus augmentation procedure, a small incision is made on the premolar or molar region to expose the jawbone. A small opening is cut into the bone, and the membrane lining the sinus is pushed upward. The underlying space is filled with bone grafting material, either from your own body or from a cadaver. Sometimes, synthetic materials that can imitate bone formation are used. After the bone is implanted, the incision is stitched up and the healing process begins. After several months of healing, the bone becomes part of the patient’s jaw and dental implants can be inserted and stabilized in this new sinus bone.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant well, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for several months, depending upon the type of graft material used. Once the graft has matured, the implants can be placed.
The sinus graft makes it possible for many patients to have dental implants when years ago there was no other option besides wearing loose dentures.
A sinus augmentation is generally performed at Dr. Graffeo and Dr. Linsky’s office, under local anesthesia. However, some patients also may request oral or intravenous sedative medication as well.
In severe cases, the ridge has been reabsorbed and a bone graft is placed to increase ridge height and/or width. This is a technique used to restore the lost bone dimension when the jaw ridge gets too thin to place conventional implants. In this procedure, the bony ridge of the jaw is literally expanded by mechanical means. Bone graft material can be placed and matured for a few months before placing the implant.
The dental specialist performs the proper treatment of facial injuries. These professionals must be well versed in emergency care, acute treatment and long-term reconstruction and rehabilitation – not just for physical reasons but emotional as well. Oral and Maxillofacial surgeons are trained, skilled and uniquely qualified to manage and treat facial trauma. Injuries to the face, by their very nature, impart a high degree of emotional, as well as physical trauma to patients. The science and art of treating these injuries requires special training involving a “hands on” experience and an understanding of how the treatment provided will influence the patient’s long term function and appearance.
Dr. Graffeo and Dr. Linsky meet and exceed these modern standards. They are on staff at local hospitals and deliver emergency room coverage for facial injuries, which include the following conditions:
There are a number of possible causes of facial trauma such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Types of facial injuries can range from injuries of teeth to extremely severe injuries of the skin and bones of the face. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels). Dr. Graffeo and Dr. Linsky are well-trained board certified oral and maxillofacial surgeon and is proficient at diagnosing and treating all types of facial lacerations.
Fractures of the bones of the face are treated in a manner similar to the fractures in other parts of the body. The specific form of treatment is determined by various factors, which include the location of the fracture, the severity of the fracture, the age, and general health of the patient. When an arm or a leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain other types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved site. This technique of treatment can often allow for healing and obviates the necessity of having the jaws wired together. This technique is called “rigid fixation” of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient’s facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary, are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Isolated injuries to teeth are quite common and may require the expertise of various dental specialists. Oral surgeons usually are involved in treating fractures in the supporting bone or in replanting teeth that have been displaced or knocked out. These types of injuries are treated by one of a number of forms of splinting (stabilizing by wiring or bonding teeth together). If a tooth is knocked out, it should be placed in salt water or milk. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible. Never attempt to wipe the tooth off, since remnants of the ligament that hold the tooth in the jaw are attached and are vital to the success of replanting the tooth. Other dental specialists may be called upon such as endodontists, who may be asked to perform root canal therapy, and/or restorative dentists who may need to repair or rebuild fractured teeth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
The proper treatment of facial injuries is now the realm of specialists who are well versed in emergency care, acute treatment, long-term reconstruction, and rehabilitation of the patient.
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs at the beginning of a pathologic process or cancerous growth:
These changes can be detected on the lips, cheeks, palate, and gum tissue around the teeth, tongue, face and/or neck. Pain does not always occur with pathology, and curiously, is not often associated with oral cancer. However, any patient with facial and/or oral pain without an obvious cause or reason may also be at risk for oral cancer.
Do not ignore suspicious lumps or sores. Please contact us so we may help.
During surgery, the BMP is soaked onto and binds with a collagen sponge. The sponge is then designed to resorb, or disappear, over time. As the sponge dissolves, the bone morphogenetic protein stimulates the cells to produce new bone. The BMP also goes away once it has completed its task of jump starting the normal bone healing process.
Since there is no need to harvest bone from the patients’ hip for BMP, recipients were spared donor site pain. Complications from the graft harvest site are also eliminated with the use of bone morphogenetic protein.
Dr. Graffeo and Dr. Linsky would be happy to discuss all grafting options with you at the time of consultation.
Crow’s feet, worry lines, and laugh lines can all be a thing of the past. These are referred to as dynamic wrinkle lines and all are treatable with this procedure. Cosmetic denervation is the process of injecting BOTOX© Cosmetic into the tiny facial muscles that create the wrinkles.
To better understand your overall health, we will evaluate your medical history prior to surgery. In addition, a complete examination of your eyes is made in order to decide the most effective injection sites. All issues and concerns will be discussed. The areas that will be treated are marked and digital photographs are taken in order to determine the amount of improvement after surgery.
BOTOX© Cosmetic injections are performed without anesthesia because they are virtually painless. Only a very small sting is felt when the injections are made. The effects are not permanent and may need to be repeated two to three times per year to retain the effects. Research has suggested, however, that long-term use of the injections leads to a longer duration of each treatment’s effect. Patients over the age of 65 may not experience such dramatic results. BOTOX© Cosmetic is only useful in treating expression lines and cannot be used to repair sagging skin caused by aging.
After the procedure patients may experience slight bruising around the area that quickly fades. Normal activities can be performed immediately. Possible side effects are temporary weakness of nearby muscles or in rare cases an eyelid may droop. BOTOX© Cosmetic is completely reversible so any side effect is only a temporary condition. The doctor will explain all risks associated at the time of your consultation.
© Westchester Oral & Maxillofacial Surgery & Implantology. All Rights Reserved. | Accessibility Policy | Privacy Policy
Last Updated: August 14th, 2023 02:50 PM